Getting more value from the imaging we already collect
How AI will change physicians and patients think about disease screening
One of the applications of AI I am most excited about is the use of AI for opportunistic screening. In short, the idea is: There is a lot of information in medical images (‘a picture is worth a thousand words’) that is captured. but not directly relevant for the reason the imaging was obtained. Such information should be fed back into the healthcare system to facilitate diagnosis and care. A canonical example could be getting a CT scan for having chest pain, and finding a lung nodule that might be early cancer.

In such an example, there is tremendous value - early identification and treatment of lung cancer can lead to improved outcomes and limit the need for toxic chemotherapies. However, there is no free lunch, as the converse downsides of such an approach is known as the incidental finding, or ‘incidentaloma’. Our bodies are imperfect, often in their own unique ways, many times without any adverse effects or impact on overall wellness, and casting a light onto those imperfects can lead to excess worry, unnecessary procedures, and inadvertent complications.
Clinical Uncertainty
In some ways, that’s a reflection back into the imperfections of medical knowledge. We simply don’t know the implications of many imaging findings and how that leads to future outcomes. Imaging has imprecision beyond variation in measuring the sizes of objects - many diseases might look very similar in a benign state and malignant states. Given the rapid cheapening and increased prevalence of medical imaging, there are many imaging findings that don’t have longitudinal follow-up or clear understanding of its implications. Many doctors are not equipped to assess the full range of imaging findings. Fun fact: After careful market landscape analysis, CT vendors intentionally narrow the field of view for CT scanners when imaging the heart for chest pain indications, in part because physicians don’t want the headache of incidental findings. [1]

Non-Opportunistic Screening
It’s in this landscape that we see some interesting applications of AI. First, there’s a camp that says we should image everything and image often, so we can better understand one’s health. In this space, there’s been a rise in many new services, from executive healthcare exams to whole body MRIs. Christina Farr wrote a thoughtful piece about the expansion of whole body MRIs as well as physicians reaction to their direct-to-consumer marketing. The physician’s reactions aren’t uniformly positive as there’s many nuanced reasons why there can be challenges and unintended consequences, but these companies claim to use AI to overcome the challenges inherent in screening and imaging. But as an AI researcher and physician, I’m doubtful at such claims.
Most such companies lack the necessary data to train AI for clinically meaningful tasks/outcomes. The exponential explosion of imaging in recent years necessitates that most imaging have been done recently. There simply isn’t as much imaging with longitudinal follow-up of outcomes to train large scale models, and the historical imaging is lower resolution and a different quality than current imaging [2]. Many datasets also lack the linkage between imaging and the eventual outcomes of the individuals scanned. Even in tasks as simple as segmentation, inevitably the challenge becomes the question of ground truth, and why we should care more about precise measurements rather than accurate measurements.
Some commentary online referred to naysayers of routine MRI screening as paternalism and gatekeeping in the healthcare industry, however I would frame it as an opinionated review. A reviewer doesn’t prevent one from buying a product, but might highlight the flaws and limitations in a way that might dissuade you from buying a product. I also think physicians are the best people to review such products as there are many technical considerations that one misses without a medical perspective. Radiologists certainly aren’t trying to limit access to imaging, but they are the best to equipped to tell you when an imaging test is insufficient and inappropriate. A whole body MRI doesn’t have enough temporal resolution to capture many cardiac abnormalities and doesn’t use contrast which is necessary to visualize many different diagnoses.
Opportunistic Screening
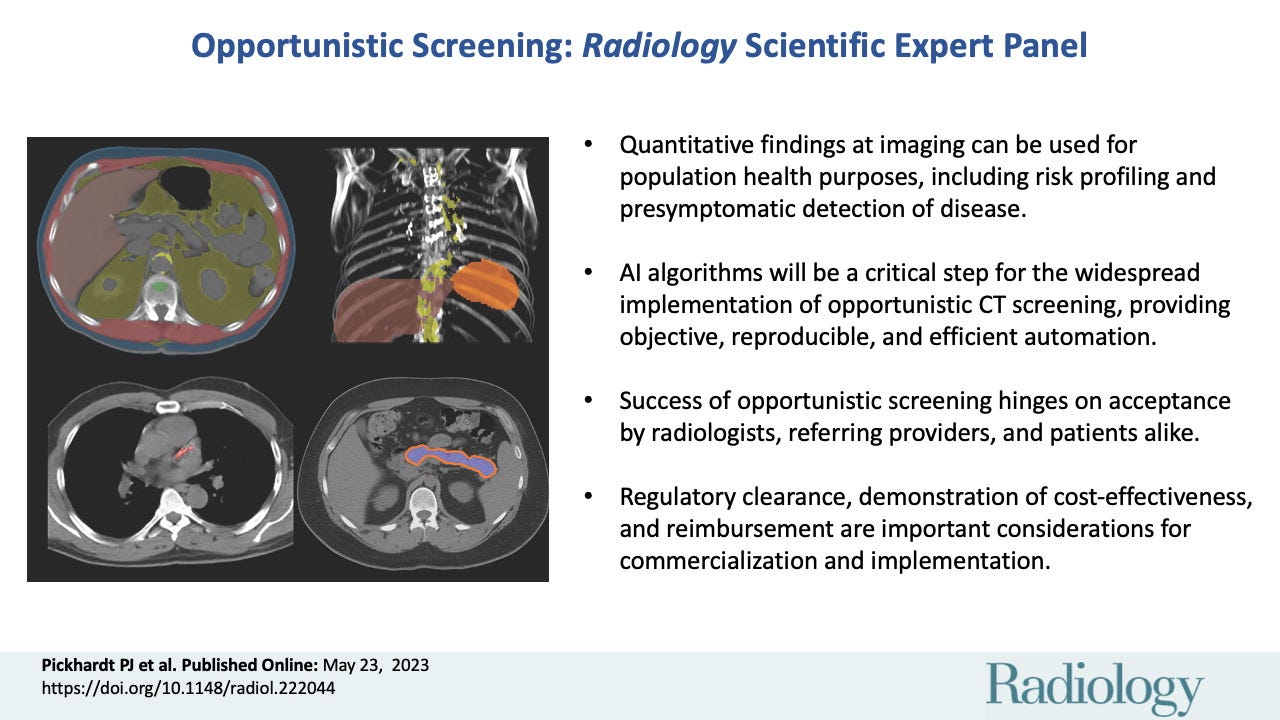
An alternative application of AI is the use of opportunistic screening. Rather than asking patients to specifically receive an imaging test (as well as the associated inconvenience and cost), what if we used AI on the routine imaging we are obtaining already? The burden of imaging is already shouldered by the fact that these test are already obtained (for whichever clinically appropriate reason they were ordered), and the opportunistic screening approach captures additional information from the data already collected.
One example I’m impressed by is the identification of incidental coronary artery calcium (no conflicts or affiliations). Coronary calcium is associated with adverse cardiovascular outcomes, and while some individuals intentional obtain specific imaging to learn this information, this information is also routinely obtained CT scans. Given that CT scans obtained for another reason are 1000x more common than CTs obtained specifically to look for coronary calcium, this is an example of useful AI surfacing already obtained data and transforming it into actionable information [3].
As I focus on echocardiography, I am particularly interested in its use for opportunistic screening. As the most common form of cardiac imaging, echocardiography is the “top of the funnel” and visualizes the wide range of patients experiencing cardiovascular symptoms and diseases. Being obtained in generally symptomatic patients, its use as a screening tool skews towards a slightly higher risk population - and improves its PPV and pre-test probability of having intervenable disease. I’m particularly interested in AI-enhanced echocardiography for diagnoses when there is an efficacious downstream treatment - such as cardiac amyloidosis or valvular heart disease (as well as other diseases which we’ll announce shortly).
The disconnect between diagnostics and therapeutics
This might seem unintuitive or controversial, but I believe the value of a diagnostic test is intrinsically linked to the potential of its downstream therapeutic options. If you can’t treat or alter the trajectory of disease A, how much value is there in its diagnosis? Screening tools are invariably tied to our ability to intervene, otherwise why screen for the disease? Pap smears lead to hysterectomies and FOBT lead to colonoscopies, but the aim of screening tests should be funnel the right patients to the right treatments. The challenge is, broadly speaking, AI technologies are diagnostic tools and not therapeutic interventions.
AI helps us better predict and quantify - and while intrinsically useful, that utility is maximized when there is a meaningful downstream treatment associated. That’s my primary critique with whole body MRI - there’s such a disconnect between diagnosis and treatment (and patients don’t recognize that), that it looks looks more and more like a false bill of goods. That’s also why I’m particularly excited about opportunistic screening - it’s minimizing the cost of detection (free when the imaging is already present) and maximizing the value of detection (by pinpoint detecting only the diseases we have treatments for).
[1] There are also modest decreases in radiation dose, but needless to say, even at the same radiation dose, there is a lot of information collected that is intentionally not reconstructed or interpreted.
[2] An AI researcher might say such data is out-of-domain, or sufficiently different that it would be hard to train a model that then generalizes well to current imaging techniques.
[3] Even when there is clear clinical value, there are important questions regarding reimbursement (who should pay?) and potential for unintended downstream consequences (does one need another dedicated study or confirm the results?).